STUDENT LIFE
-
Student Life
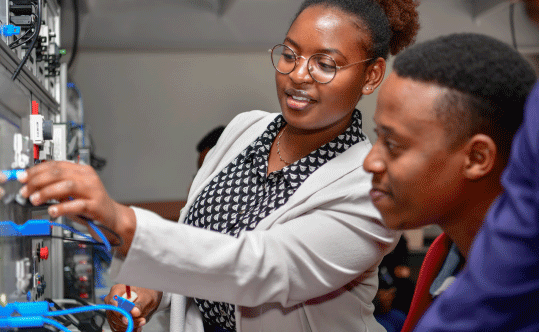
The student life at Strathmore University is vibrant and diverse, providing students with opportunities for academic excellence, personal growth, and social engagement.
-
MENTORING SERVICES
The mission of Strathmore University is to provide an all-round quality education where students get professional training and acquire the personal qualities and necessary preparation to be responsible citizens, with values such as good conduct and hard work.
-
HEALTH AND WELLNESS
The goal of Strathmore University Medical Centre is to deliver comprehensive quality care that is accessible, affordable, available and patient-centered that meets internationally accepted standards
SHORT COURSES / EVENTS
Events
Schools
-
Strathmore Institute of Management and Technology (SI)
Access
-
Strathmore Institute of Mathematical Sciences (SIMS)
Access
-

School of Tourism and Hospitality (STH)
Access
-

School of Humanities and Social Sciences (SHSS)
Access
-

Strathmore Law School (SLS)
Access
-

Strathmore Business School (SBS)
Access
-

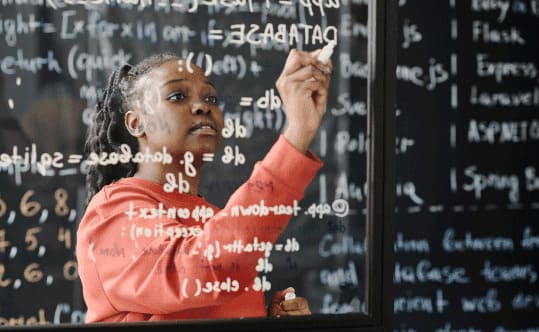
School of Computing and Engineering Sciences (SCES)
Access
Are You...

STRATH VOICES
-

“I got guidance, built networks, made friends who are now a close
Anna Jessica
-

“This community has been instrumental in my academic journey. I’m grateful for
Simon Bakibinga
-

“My journey at Strathmore University was a riveting ride of self-discovery and
Susan Waweru
-

“I’ve always had a strong love for mathematics and business; actuarial science
Irenee Vunabandi
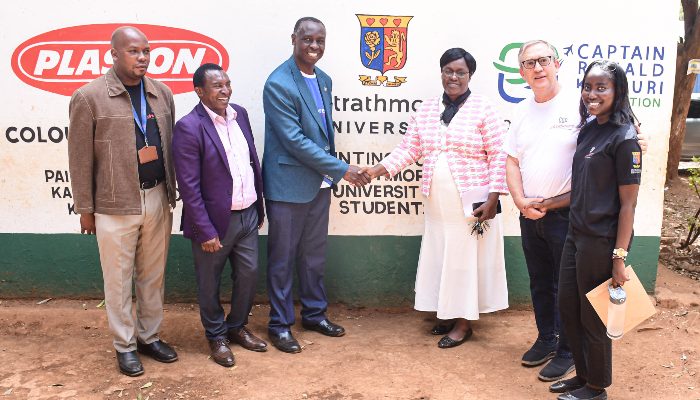
PARTNERS